Dental Implants
A Tooth-Replacement Method That Rarely Fails
(Continued)
Later Failures
There are two primary reasons for “later” implant failure after the osseo-integration process has been successful. These include over-stressing implants with too much biting force, or inflammatory disease of the gum tissues and/or bone around the implant.
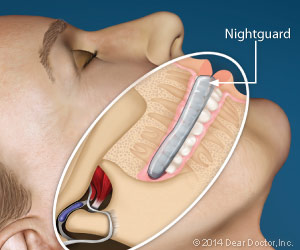 |
| A biteguard is often recommended to protect not only implants but also the natural teeth for people who have clenching or grinding habits that are difficult to control, particularly at night. |
Overloading Implants
If you have a teeth grinding or clenching habit, your dentist will probably recommend a nightguard to wear while you sleep so that your implants are not over stressed. Occlusal (bite) overload (excessive force) may result in implant failure: either through bone loss occurring around the implants; the crowns may either wear or break over time; or occasionally the implants themselves may fracture. This is less common today than it was when implants came in only one size and shape and were made out of pure titanium. Today, all metal implants are made of a titanium alloy, which is much stronger. Thanks to experience and research, we now have implants of varying sizes and shapes (usually cylindrical or tapered), that can be used to replace different shapes and positions of teeth. Larger implants are also manufactured to replace back teeth, to handle the increased biting forces that are applied in the back of the mouth.
Inflammatory Disease Around Implants
Inflammation and infection of the surrounding living tissues that support implants is perhaps the greatest cause of concern today regarding implant failure. It is generally referred to as peri-implantitis (“peri” – around; implant “itis” – inflammation).
Gum Inflammation. The first phase of peri-implantitis is a condition in which the soft gum tissues surrounding the implant become inflamed or infected. This can happen when excess dental cement (used in some cases to attach a crown) is not completely removed from beneath the gum line; or, more commonly, it can result from biofilm (bacterial) accumulation. If inflammation/infection is limited to the gum tissues, removing any excess cement and/or improving oral hygiene, and cleaning to remove biofilm, can generally manage it. It is also important for the implant surgeon to make sure that the implant is surrounded by sufficient gum tissue; gum tissue tightly adheres to the implant or implant crown surface, providing a barrier to food debris penetrating below the gum line. However, it may not prevent inflammation from biofilm bacteria.
Bone Inflammation. Inflammation/infection extending into the bone destroys the connection between the implant and the bone and is therefore much more problematic. It undermines the support for the implant, and hence the tooth root and crown that it replaces. Peri-implantitis often has the usual signs of inflammation: redness, swelling, bleeding and suppuration (pus formation) in the peri-implant tissues. However, symptoms may vary: It’s possible to have mild symptoms or even none at all in chronically infected sites, to acute painful abscesses. In more severe cases, bone loss can be rapid and ultimately an implant can loosen and be lost. It has been speculated that individuals who had prior periodontal disease, which resulted in their tooth loss, would be at greater risk for peri-implantitis, but this does not generally seem to be the case.
Peri-implantitis can be treated successfully if caught early enough. It requires control of the inflammation/infection with local cleaning or antibiotics. Attempts at surgical repair may be necessary to regain attachment and bone. The biggest problem is decontaminating the exposed implant surfaces. This is difficult because they are intentionally microscopically roughened to aid attachment to the bone. If an implant is lost due to peri-implantitis every effort is made to preserve the surrounding bone and replace the implant.
Maintenance Is Your Best Protection
Prevention pays great dividends in avoiding implant failure. Once the implants are placed, the ball is largely in your court. It’s crucial to maintain a good oral hygiene routine. Make sure you have regular professional dental cleanings to help keep the tissues around your implants healthy. Routine maintenance for implants is really no more difficult than it is for natural teeth. If it were, success rates for this life-changing tooth-replacement treatment would not be nearly so high. And if a problem develops, it is best solved by early recognition and treatment.





