Periodontal Flap Surgery
How Periodontal Surgery Can Save Your Teeth
(Continued)
Where The Action Is — Inside The Flap
When the surgical area and root surfaces are thoroughly and scrupulously cleaned to remove any diseased tissue, attention can then be paid to the root surfaces and the bone. Today's regenerative techniques take into account wound healing studies and knowledge of the cell types that allow for the creation of new periodontal ligament tissues that attach to the tooth root.
The periodontal ligament attaches the tooth root to the supporting bone. It is comprised of:
- Cementum, a cement-like substance.
- Periodontal ligament fibers, made of collagen, which embed into the cementum of the tooth root.
- Bone of the tooth socket, to which the fibers of the ligament connect.
The periodontal ligament suspends the tooth in the bone in a hammock-like arrangement. With today's technology, all lost components of this system can be regenerated.
The beauty and essence of the flap approach is that it maintains and preserves the existing healthy outer layers of gingival tissue while allowing access to remove diseased tissue lining and regenerate new tissue within.
The Root Of The Problem
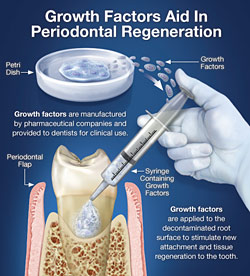
Much attention has been paid to the management of root surfaces, the focus of years of periodontal research. The general consensus is that the roots must be diligently cleaned, using a process generally known as root planing or debridement, and sometimes further managed by etching with special root surface conditioners or antibiotics like tetracycline. Only when free of contaminants can new tissues grow and reattach to root surfaces. When the inside of the flap and roots are freshly cleaned “growth factors” can be used to stimulate and enhance healing.
Growth factors have been used successfully to stimulate the formation of new periodontal ligament in humans.
 |
| Growth Factors Aid In Periodontal Regeneration
Click to enlarge |
Careful research has demonstrated that these naturally occurring substances, also known as cytokines (“cyto” – cell; “kine” – movement), are capable of stimulating remarkable healing activities. In simpler words, they transform and heal into new and specific tissues. For example, proteins called amelogenins (“amelo” – enamel; “genin” – generating) aid in new periodontal tissue regeneration. They are produced during the development of teeth and formation of the periodontal ligament when teeth are newly erupting. When placed directly on to specially treated root surfaces, they have been used successfully to stimulate the formation of new periodontal ligament. Platelet-derived growth factors PDGFs, come from the small, plate like free-floating particles in blood that help blood clot and stop bleeding. They liberate powerful growth enhancing factors that also can be used to stimulate and promote periodontal wound healing.
Wound Healing
As can be seen from the examples, an understanding of the process of how wounds heal, is clearly critical to achieving successful surgical results. More recently basic science has demystified wound healing with a detailed understanding of cellular and growth factors. The process of inflammation, the body's most basic evolutionary response to injury and infection, causes the attraction of stem cells and liberation of growth factors — a veritable treasure chest of “magical molecules” that initiate and promote wound healing. The ability to isolate these substances, determine their roles, and then synthesize or manufacture them has allowed periodontal and other surgical specialists to hasten wound healing as well as regenerate tissues. As a result healing is uneventful and results are more predictable.



