Seeking Relief from TMD
What You Should Know About Treatment For Temporomandibular Disorders (TMD)
(Continued)
Potential TMD Symptoms
Obviously, you don't want to make a TMD diagnosis on yourself without professional counsel, but it is helpful to know the classic symptoms (which a patient notices) and signs (which a dental professional notices) that might suggest a potential TMD problem:
Because there are different approaches to the management of TMD problems, not all of which are based on science, caution is advised when seeking professional help.
Clicking: The first issue is a clicking sound coming from the TMJ, which usually is due to a shift in the position of the disk inside the joint. This usually can be heard by you, the patient or even by somebody standing nearby, and it can be felt with the fingers placed on your face in front of the ears. However, this can be a good example of an insignificant symptom if you do not also have pain or limited jaw function. Research has shown that over one third of the world's population has one or both TMJs that “click,” so it is pretty clear that clicking alone is not an important abnormality for most people. Most TMJ “clickers” never progress to having significant symptoms, and in many cases the clicking diminishes or goes away entirely. Therefore, asymptomatic clicks (“a” – without; “symptoms” – pain or discomfort) do not require treatment. Clicks with pain, on the other hand, are a subtype of TMD, and these are referred to as internal derangements of the TM joint. Other symptoms may include the jaw getting “stuck” in open or closed positions. These conditions require professional attention.
Muscle Pain: The second issue is symptomatic jaw muscle pain, which is usually felt in the cheeks (masseter muscles) and temples (temporalis muscles), where the two big pairs of jaw-closing muscles are located. The simplest version of jaw muscle pain is soreness and stiffness in the morning. This usually is related to parafunctional nighttime habits (“para” – outside; “function” – normal range), such as clenching and/or grinding of the teeth. This can usually be easily managed by wearing a customized and properly adjusted oral appliance (nightguard). However, there are other jaw muscle conditions that produce painful scenarios that are much more complicated, and the pain may spread (via shared nerves) to nearby head and neck areas. These more complex TMD conditions do not respond well to wearing nightguards, and accordingly more complex treatments administered by experienced and well-trained professionals are usually required.
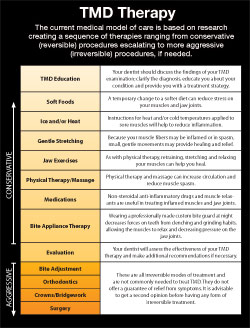
The current medical model is based on the proposition that the TMJ is a joint and has much in common with any other joint.
True Temporomandibular Joint Pain: The third issue is pain actually inside one or both jaw joints, which technically is described as arthritis (“arth” – joint; “itis” – inflammation) of the TMJ. Interestingly, many people have arthritic-looking TMJs if radiographs (x-ray pictures) are taken, but they may have no symptoms of pain or dysfunction; others have pretty significant symptoms of pain and dysfunction, but their radiographs look normal. Since there is no cure for arthritis anywhere in the body, people afflicted with TMJ arthritis should expect fluctuations in their arthritic symptoms. Their pain often can be treated conservatively and/or self-managed with non-steroidal anti-inflammatory medications, rest, soft diet, and physical therapy. Severe cases will require more complex forms of professional care, which in a few cases may include minor procedures inside the joint such as cortisone injections or lavage (flushing) of the joint. Major surgeries are rarely necessary for TMD.
The Often Confusing World Of TMD Treatment
So let's assume that you or somebody you care about has developed a problem of what seems to be jaw pain and dysfunction — what should you do? Of course you should probably start with a visit to your family doctor to rule out medical conditions that cause head and face pain, some of which can mimic a TMD. Next, you should see your family dentist, who will either offer to treat you or to refer you elsewhere. This is where you, as the consumer/patient, will need to be well-informed about the current controversies that exist in the TMD field. Simply stated, the TMD field today is in transition between a traditional dental model and a contemporary medical model, and this has tremendous implications for what will happen to you as you seek a proper diagnosis and treatment.
 |
| TMD Muscle Pain Cycle
Click to enlarge |
The (old) dental model was based on theories such as malocclusions (“mal” – bad; “occlusion” – bite) causing jaw muscle pain, or missing teeth causing jaw dysfunction, or some kind of jaw mal-alignment causing disks to slip out of place and produce pain in the joints. These concepts inevitably led to a “need” for mechanical corrections to be made, which would be accomplished by orthodontics (braces), crowning teeth, or making bite adjustments by grinding (reshaping) the teeth. These procedures are irreversible, and so in many ways they are similar to surgical treatments. However, research from around the world in the last 25-30 years has shown that these mechanistic concepts about TMD treatment are largely unfounded, and therefore these kinds of irreversible treatments are generally not necessary.
The current medical model is based on the proposition that the TMJ is a joint and has much in common with any other joint. Therefore, it can be subject to all sorts of typical orthopedic problems — sore muscles, inflamed joints, strained tendons and ligaments, and of course disk problems. Almost all of these problems are capable of being treated without permanently changing or altering the joint structure/s. Obviously, in this model the “alignment” of teeth and jaws is neither analyzed nor changed because those factors have been proven to be mostly irrelevant to what is causing the TMD symptoms. Thus, the medical model is also more conservative, and patients treated within this framework can be spared the more invasive and expensive dental procedures of the past. Additionally, TMDs are now known to be influenced by genes, gender, and age, as well as a host of environmental and behavioral triggers such as stress and anxiety. For many patients, jaw pain may be a manifestation of a larger medical malady, including other widespread pain-inducing conditions such as fibromyalgia (“fibro” – connective tissues; “myo” – muscle; “algia” – pain). These new discoveries make it even more important to deal with TMDs within a medical framework.
The American Association of Dental Research (AADR) regarding Temporomandibular Disorders (TMDs) concludes: “It is strongly recommended that, unless there are specific and justifiable indications to the contrary, treatment of TMD patients initially should be based on the use of conservative, reversible and evidence-based therapeutic modalities. Studies of the natural history of many TMDs suggest that they tend to improve or resolve over time. While no specific therapies have been proven to be uniformly effective, many of the conservative modalities have proven to be at least as effective in providing symptomatic relief as most forms of invasive treatment. Because those modalities do not produce irreversible changes, they present much less risk of being harmful. Professional treatment should be augmented with a home care program, in which patients are taught about their disorder and how to manage their symptoms.”
I hope this information about temporomandibular disorders will prove to be helpful to you or somebody you care about. Importantly, for individuals who continue to have TMD problems even after good conservative treatment has been provided for at least several weeks, or if the symptoms are progressively getting worse, further diagnosis and treatment should be sought at a dental college or hospital which has an Orofacial Pain clinic. Should a TMD problem arise, the resources listed below can be helpful.
Continue reading TMD Questions To Ask Your Dentist

