Root Cavities
Tooth decay near the gum line affects many older adults
Dear Doctor,
My dentist just told me I have a “root cavity” that needs treatment soon. But I am over 60 years old and none of my teeth hurt me. What's going on here?
Dear Steven,
The problem you are experiencing is common among seniors. The reason it needs treatment soon is that decay on the root of a tooth can spread inside the tooth more rapidly than a cavity on the crown surfaces. Let's examine the anatomy of a tooth to see why this is so.
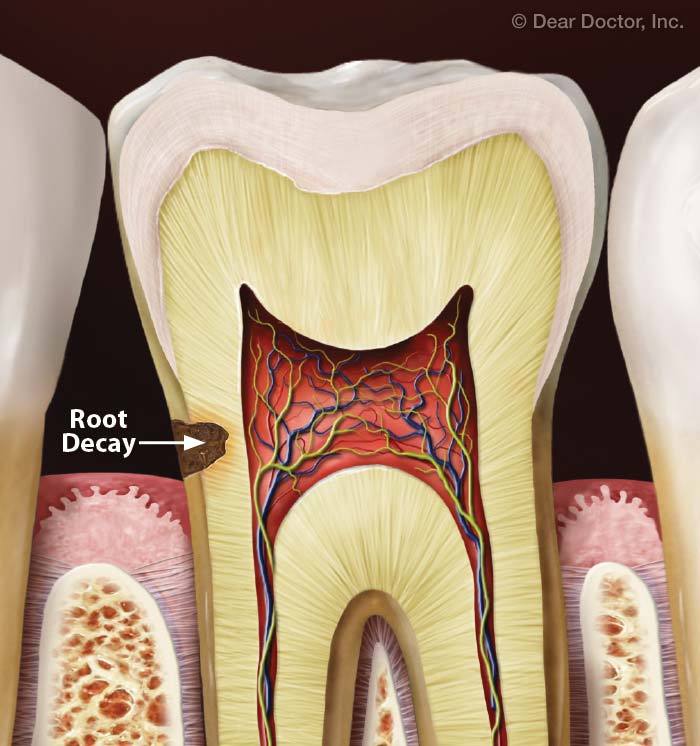 |
| Exposed root surfaces are more vulnerable to decay, which is shown forming in this tooth. |
The pearly whites you see when you smile are the crowns (upper portion) of your teeth. Beneath your gums, the roots of your teeth extend into your jawbone and provide the support needed to keep your teeth firmly in place. Crowns and roots have very different outer surfaces: crowns have a shiny hard covering called enamel, the hardest and most highly mineralized substance in the human body. The roots are covered by a thin layer of cementum, a dull yellowish mineralized substance, that is much softer than enamel.
Root cementum doesn't offer the same level of protection from decay-causing bacteria and erosive acids in the diet that enamel does. While tooth roots are usually protected by gum tissue that covers them, this is not always the case. Many people, particularly seniors, experience receding gums, where the smooth, pink tissue surrounding the tooth roots is positioned lower down the roots, exposing parts of the root surfaces. Common causes of gum recession include gum disease and related bone loss, overly aggressive tooth brushing, and poor tooth position.
Exposed tooth roots can create a cosmetic problem if you don't consider the yellowish color of cementum attractive in your smile. More importantly, root exposure can become a health issue when, as in your case, the unprotected root surface develops a hole (cavity) that can worsen in a rather short period of time. Cavities form when acids in the mouth start to dissolve (demineralize) the tooth structure. These acids mostly come from two sources: oral bacteria, which produce acid in the process of breaking down the sugar that sustains them; and/or acidic foods and beverages such as soda (both regular and diet) and fruit juices.
As a cavity forms, bacteria move further inside the tooth and cause more rapid demineralization as they remain shielded from your hygiene efforts and dissolve more layers of tooth structure. Left untreated, the decay can spread all the way into the tooth's inner pulp (nerve) tissue — and if that happens, you will probably need root canal treatment, or possibly need the tooth removed. This decay process moves a lot faster when there's no enamel barrier — and faster still when a person has a problem with dry mouth. That's because saliva is a natural cavity-fighter that neutralizes acid and replenishes minerals that have dissolved out of the teeth.
Treating a cavity on an exposed part of the tooth root involves removing decay with a dental drill and placing a filling. Occasionally, root decay can progress below the gum line. When that happens, minor gum surgery may be needed to gain access to the decayed area.
As part of your treatment, your dentist may apply fluoride varnish onto your teeth for added protection against cavities. The fluoride gets incorporated into the tooth structure, making it more resistant to tooth decay. Fluoride rinses you can use at home may also be recommended.
While we're on the subject of at-home care, let's remember that everyone has a role to play in keeping their teeth strong and healthy. Along with using preventive rinses or other hygiene aids your dentist may recommend, make sure you are brushing twice each day with a soft-bristled toothbrush to remove dental plaque (a white bacterial film that develops on teeth), and that you brush all the way to the gum line. Use small, gentle circular motions with the toothbrush and avoid harsh scrubbing as this may damage your gums. It's also important to floss at least once a day, so you can remove plaque from between the teeth, where a toothbrush can't reach.
It may also be a good idea to consult with your dentist or physician about adjusting your medications if they cause dry mouth, so they have less of an impact on your oral health.
Keep sugary, sticky and acidic foods out of your diet as much as possible because sugar increases the risk of decay. This includes hard sugar candies used to stimulate saliva flow and relieve dry mouth. Make sure any lozenges you use for this purpose are sugar-free, and ask your dentist to recommend other products that can help relieve mouth dryness if this is a problem for you. It may also be a good idea to consult with your dentist and physician about adjusting your medications if they cause dry mouth, so they have less of an impact on your oral health.
With appropriate oral care at home and at the dental office, your natural teeth can serve you well for many years to come.

