Root Canal Treatment
What You Need to Know
 |
If you've been told you need a root canal, you may be feeling a little apprehensive. After all, everyone's heard the old cliché, "I'd rather have a root canal." Is it really that bad? In a word, no. We have a lot of information to share with you about this tooth-saving procedure, but here's the main takeaway: Root canal treatment is nothing to fear. Really!
 |
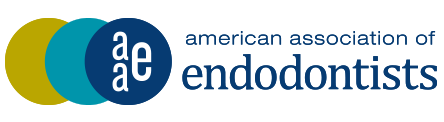
| Figure 1: Normal anatomy of the pulp chamber and root canals. (Click to enlarge) |
 |
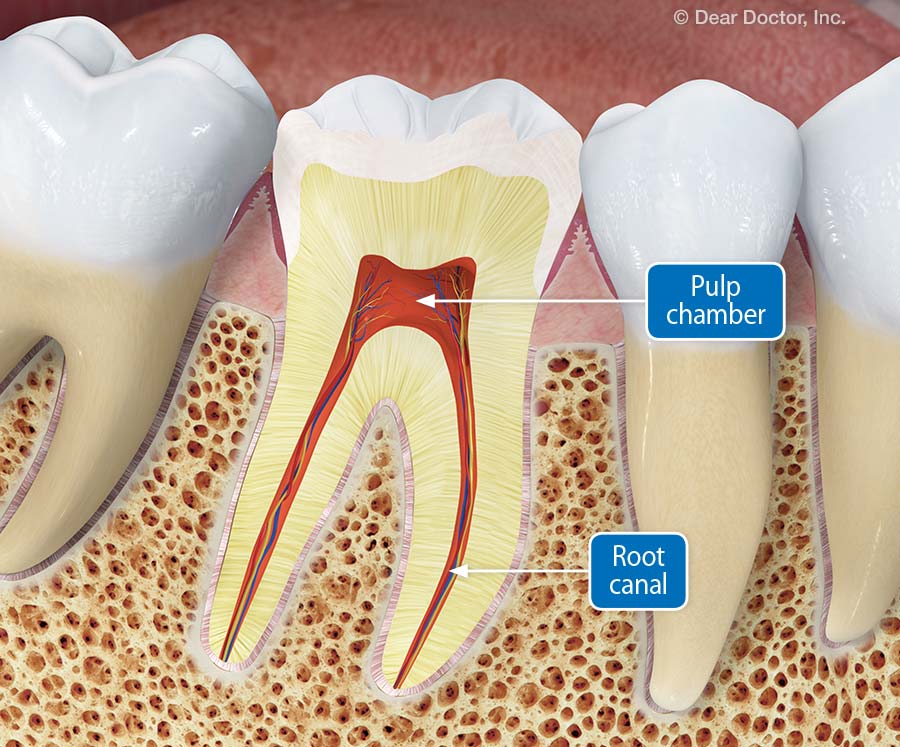
| Figure 2: The tissues within the pulp chamber and canals can become infected from the same bacteria that caused the tooth decay. (Click to enlarge) |
Why Is It Called "Root Canal"?
The term "root canal" actually has two meanings. It is commonly used to describe a procedure for treating inflammation or a bacterial infection deep inside a tooth, as in "you need a root canal." And it is also the name of a part of the tooth itself: the narrow, hollow channel that runs from the tip of the root to a central space in the center of the tooth called the pulp chamber (figure 1).
These inner tooth spaces house the nerves and blood vessels that nourished the tooth as it was growing. In adults, these tissues aren't really needed — but they do allow the tooth to feel pain, hot, cold and other stimuli. A front tooth that has one root will have one main canal. A molar, which has multiple roots, will have more than one canal. A main root canal can have several "accessory" canals branching off of it.
The tissues within the pulp chamber and canals can become inflamed or infected by bacteria; this sometimes happens when a cavity is not treated in a timely manner, or when a tooth is injured (figure 2). The inflamed tissues often cause pain inside the tooth. The purpose of root canal treatment is to relieve the pain and stop the infection.
It's also possible to have a root canal problem without pain. But if your dentist has identified a root canal infection, you need to get it taken care of — right away. If you don't, sooner or later you will likely lose the tooth. Without treatment, the infection could get worse.
 |
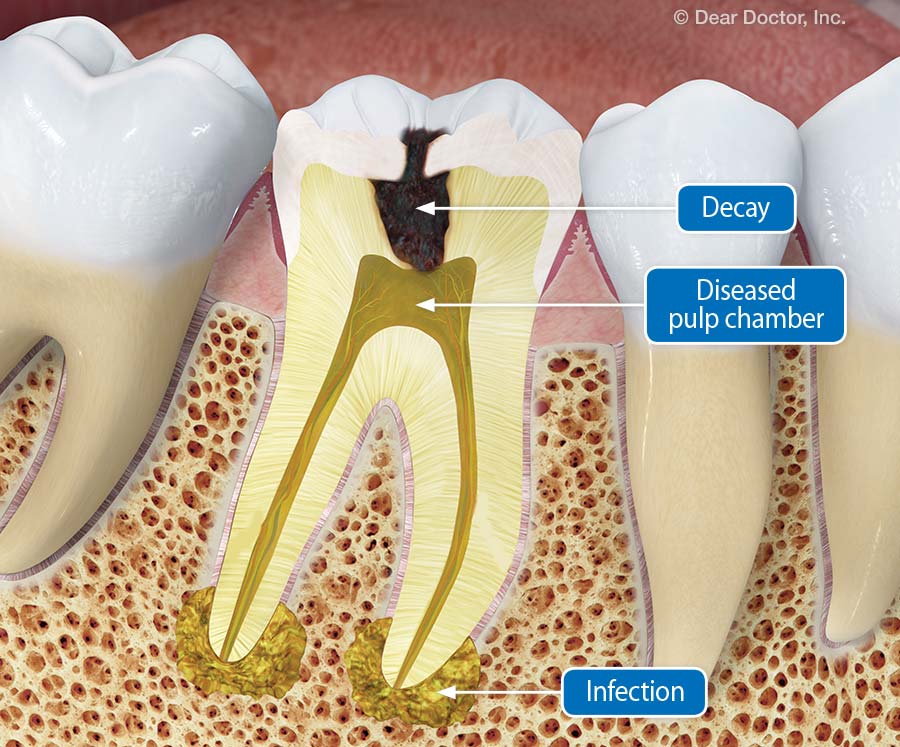
| Figure 3: A root canal in a molar is more difficult because of longer roots and multiple canals, which often have accessory canals. Endodontists are specially trained to handle this type of situation. (Click to enlarge) |
Who Performs Root Canal Treatment?
All general dentists receive training in root canal treatment, but the dental specialty devoted to it is called Endodontics ("endo" – inside; "odont" – tooth). Endodontists complete at least two additional years of training in root canal procedures after graduating from dental school to become experts in performing root canal treatment and diagnosing and treating tooth pain. Many general dentists prefer to send patients needing root canal treatment to an endodontist, particularly if the infected tooth has multiple roots and accessory canals (figure 3).
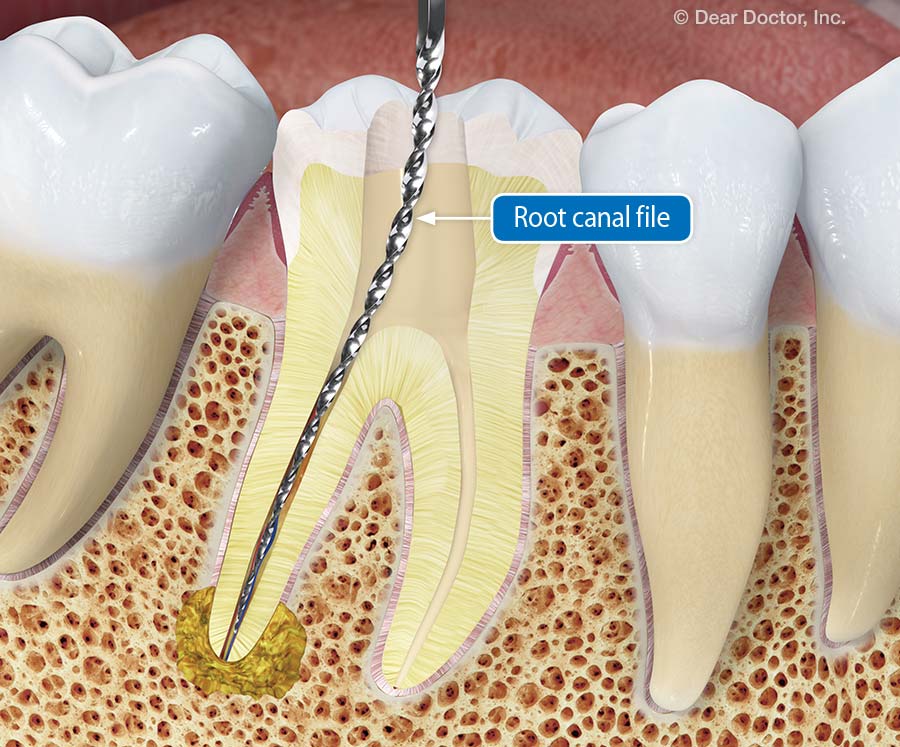 |
| Figure 4: Specially designed instruments are used to remove the diseased pulp tissue. (Click to enlarge) |
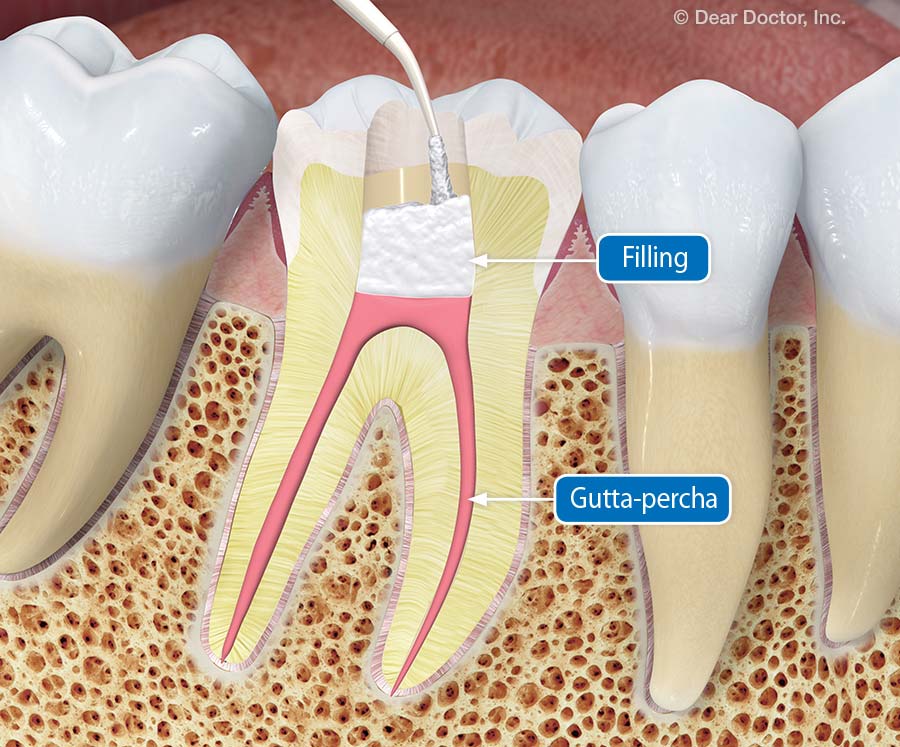 |
| Figure 5: The canals are filled with gutta-percha which seals them up and prevents bacteria from re-entering the tooth. A filling material seals the tooth until the final crown is placed. (Click to enlarge) |
What Happens During a Root Canal Procedure?
The goal of root canal treatment is to remove all diseased tissue from inside the tooth, and to seal the tooth against re-infection. The first step is to make you comfortable with local anesthesia. A thin sheet of vinyl or rubber called a dental dam will be used to keep the area around the affected tooth isolated and dry during the procedure.
In order to reach the infection, a small access hole will be drilled in the tooth — through the biting surface of a back tooth or the back side of a front tooth. Specially designed instruments will be used (frequently with a microscope) to remove the tooth's diseased pulp (figure 4). You won't feel this because the area will be numb. An added bonus is that once this tissue is gone, the tooth will no longer be able to feel pain.
Next, the canals will be flushed with antibacterial solutions, and then filled completely with a rubberlike biocompatible material called gutta-percha. The gutta-percha will be sealed into the tooth with adhesive cement, and then the access hole will receive a filling. These fillings and sealers will prevent bacteria from once again entering the tooth (figure 5).
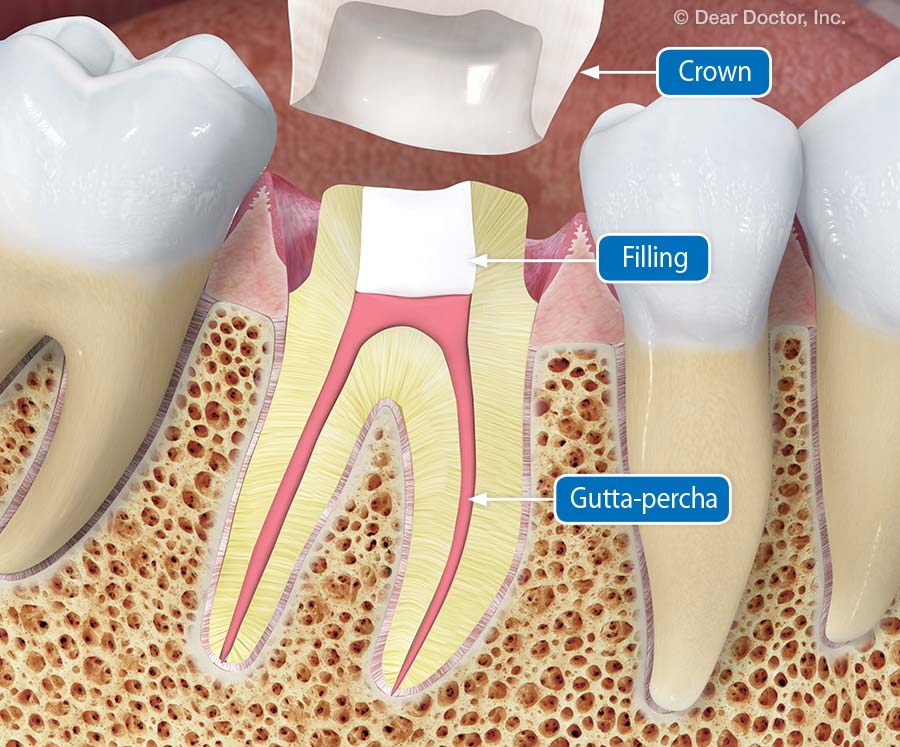 |
| Figure 6: The tooth is prepared to receive a full crown. (Click to enlarge) |
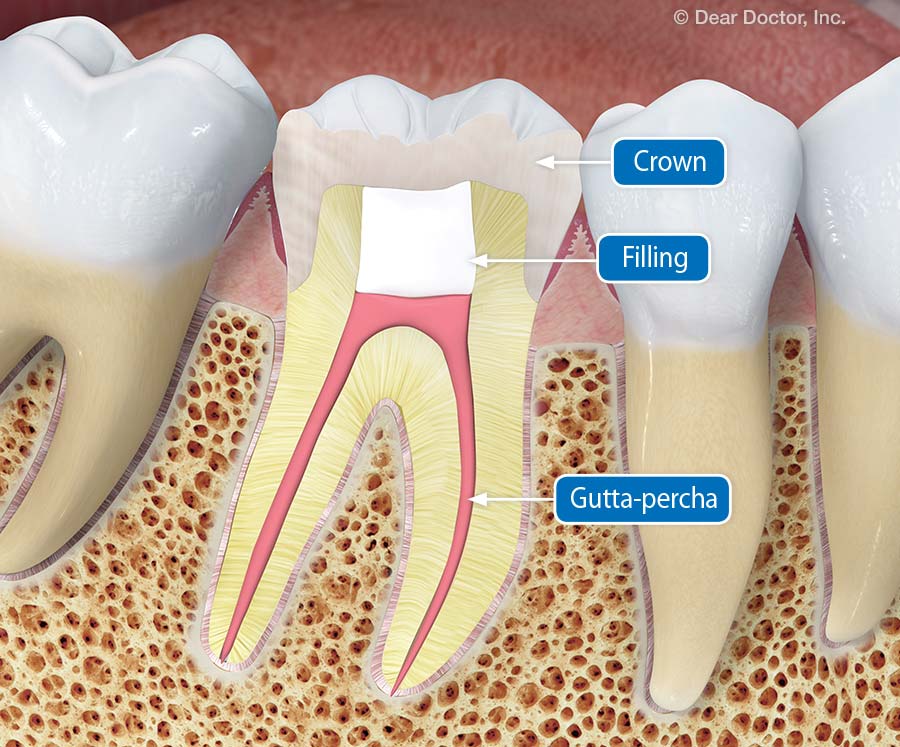 |
| Figure 7: A crown is used to protect the tooth from future fracture or damage. (Click to enlarge) |
What Happens After a Root Canal Procedure?
It is normal to experience some minor soreness for a few days after a root-canal procedure — but no more than you would expect from an ordinary filling. Any discomfort can usually be managed with over-the-counter medications such as ibuprofen.
If you were referred to an endodontist, it is likely that you will need to return to the dentist in a few weeks to receive a more permanent filling for the access hole. Most often, a full-coverage dental crown is recommended to completely seal the tooth and prevent it from fracturing under stress (figure 6 and 7). This is especially helpful in back molars, which receive the most biting force. When properly restored, a root-canal-treated tooth can last for a lifetime.
Root canal treatment is a highly successful procedure that has enabled millions of people around the world to keep teeth that would otherwise have been lost. It can also save thousands of dollars in tooth-replacement costs. Wouldn't you rather have a root canal?